 |
|
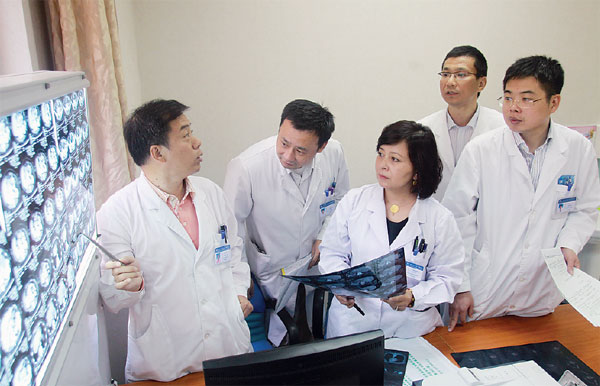
Jiang Liming (first left), Yihebali Chi (center), Zhao Hong (first right) and colleagues at the Cancer Hospital of the Chinese Academy of Medical Sciences hold a Multiple Disciplinary Treatment session on neuroendocrine tumors. Zou Hong / China Daily |
"Although the patient is still the focal point, communication must be conducted directly among the doctors, because they are on the same platform professionally," she said. "To let a patient speak separately with every one of his or her doctors totally misses the point. Crucial information may be withheld, and the clash of ideas that could lead to a potentially better solution would be impossible. Very often, the patient is left with piecemeal advice from various doctors, but is incapable of drawing any conclusion from it."
The impact of the lack of communication could be irreversible when it comes to tumor treatment, according to Zhao Dongbing, a specialist in abdominal surgery at the Cancer Hospital of the Chinese Academy of Medical Sciences.
"Drafting a well-informed treatment plan to ensure that the right thing is done at the right time requires teamwork. For that reason, MDT should start at the beginning of a patient's battle with the disease," he said.
Zhao's hospital was one of the first in China to implement MDT. "The physicians tried to incorporate the concept into daily operations when the hospital was founded in 1958, but it's only in the last decade that the hospital started to embrace it more thoroughly and systematically," he said.
Overcoming limitations
On Sept 25, Zhao Hong, a colleague of Zhao Dongbing, and three colleagues who specialize in internal medicine, interventional surgery and medical imaging, were scrutinizing CT scans and MRI slides against a bright screen. The patient, Xu Yeli, from the Inner Mongolia autonomous region, had come for treatment of a neuroendocrine tumor in her pancreas. "We looked in vain across the (autonomous) region for six months, trying to find a hospital that could treat my wife," Kang Xiaoyong, Xu's husband, said.
"For genuine discussions to take place, all MDT participants must be experts in their own field. That's the only way to avoid embarrassment and the resultant withholding of ideas," Zhao Hong said. "But, the national health authorities have made it very clear that only chief or associate chief physicians or surgeons are entitled to take part in MDT sessions. That means an MDT for neuroendocrine tumors is impossible in most Chinese hospitals because the disease is rare, so there aren't enough doctors qualified to discuss it."
To overcome the problem, the CAMS' cancer hospital is one of the few in China to operate what Ren Hua, a radiation oncologist at the hospital, described as a "tumor board".
"Unlike consultations in outpatient clinics, a tumor board is a closed-door form of MDT in which only doctors participate. They are conducted in most cancer hospitals in the US on a regular basis," said Ren, who trained at the Houston Methodist Hospital in Texas. "When you've been a doctor for some time, you understand that the absence of a patient is often conducive to the discussion of his or her disease."
According to Ren, doctors in the US are more straightforward about expressing their views, partly because they are affiliated with, but do not "belong" to, hospitals in the way their Chinese count-erparts do. "Therefore, they can afford to risk interpersonal relationships sometimes," he said.
That consideration led Yihebali Chi, the physician who leads the hospital's neuroendocrine tumor board, to place team building at the heart of the group's efforts.
"An MDT, or tumor board, is about much more than just putting some specialists together. It's about forming a team and forging a tight and trusting working relationship among its members that can make open, and sometimes difficult, exchanges possible," said Chi, a member of the Uygur ethnic group. "Rather than offering opinions to one doctor who takes main responsibly for the patient, we bear equal responsibility and work toward a common goal."
Set up in 2011 by many of the medics involved in the MDT for the disease, the neuroendocrine tumor board meets monthly and about 10 cases are put up for discussion during each session, which can run as long as four hours. "Only a doctor can submit a case. We want to make sure the most complex cases get the attention they are due," said Zhao Hong, who is also a member of the board.
Jiang Liming, a physician who works as a radiologist on Chi's team, said tumor boards makes the best use of the pooled resources. "A radiologist shouldn't just sit in his or her own small room, scan the patient and write an opinion in less than three lines. When necessary, he or she should voice observations and judgments directly to other doctors, who otherwise may only see those few lines," he said.
"However, in addition to the actual discussion time, one also has to go through all the medical records to prepare beforehand. It's really time-consuming and we aren't paid for our involvement. Consequently, many colleagues are still very reluctant to join. However, I believe they would get involved if they learned about the real benefits," he said. "The tumor board is not only a problem-solving platform, but also a training ground for doctors. Being challenged makes one think harder and raise one's performance."
Chi said the patients and their families are always informed of the results of the deliberations. "Sometimes, the discussions yield a clear solution or plan, but at other times there can be more than one way to go. We let the patient make the final choice," she said.
"The tumor board is a grassroots initiative. The MDT wasn't founded by the hospital authorities - we doctors sat together and said we wanted to do this. So we did it, and are continuing to do it. We genuinely hope that others will be inspired and follow suit," she added.
Obstacles
Inspiring others may be hard work, though. Liu Duanqi, who has served on several MDT boards, said many were convened simply because the patients was important. "The overwhelming majority of the MDT boards took place not because of the disease, but because the patient was very well-connected," he said.
Qin, from the Beijing Haidian Hospital, said China's medical system is an obstacle to MDT for cancer patients. "Our system is not patient-oriented. The doctors sit where they are, while the patients run around," he said. "The introduction of MDT on a larger scale would require a fundamental change in policies and our way of thinking."
Ren said the United Kingdom's National Health Service began promoting MDT in the 1990s, having noticed a marked difference in the effectiveness of cancer treatments in the UK and in Continental Europe, where MDT was already being used.
"Ultimately, treating cancer is about treating a diseased body as a whole. If we don't take it as a whole, we lose the battle," he said.
And it's not just about the body, according to Qin. "MDT is more than a medical procedure. At its heart, it's a form of philosophical thinking that refuses to regard a human being and his or her body as a machine," she said.
"If a machine breaks down, you can replace the damaged part and it will start working again. The human body is not the same. Whether it stands a chance of bouncing back or not, it deserves gentle, holistic care that conveys the spirit of modern medicine."
Contact the writer at [email protected]
